Undersea and Hyperbaric Medicine (UHB) – Diving Medicine
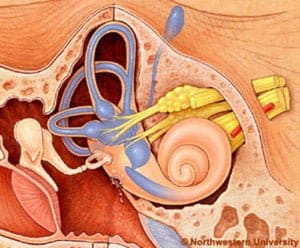
Free diving and underwater hunting are activities that require good physical condition and excellent function of the ears, nose and sinuses, the air cavities that are located in our head.
Free diving and underwater hunting are activities that require good physical condition and excellent function of the ears, nose and sinuses, the air cavities that are located in our head.
Specialisation
Dr. Dimitris Louloudis has been specialized in diving medicine at the Athens Naval Hospital. He has a 3rddegree Diploma for Free Diving from FDI, a 2nd degree Diploma for Scuba Diving from the Navy’s Underwater Disaster Unit and is also an passionate underwater hunter. He has been dealing with otorhinolaryngological (ΕΝΤ) diving problems since 1990.
He has published dozens of articles in the special press on medical issues related to diving and have given an equal number of lectures at free and scuba diving events and underwater hunting.
In addition, the doctor has been participating in a research project in collaboration with the Medical School of Harvard University in Boston, USA, since the beginning of 2008, for the treatment, pharmaceutical and surgical problems of the eustachian tube.-Sudden Deafness – Diving and spearfishing, Eustachian Tube, Frontal/ Forehead Balloon, Equalization Methods
Blocked Ear After Diving, Paranasal sinuses, The Messages of Our Body
As sudden deafness, we characterize the situation where we lose at least 30 dB of hearing (dB = decibel = sound intensity unit) in 3 consecutive frequencies over a period of less than 3 days. It is usually a unilateral condition. Its incidence is estimated at 5-20 new cases per 100,000 inhabitants per year, although it may be even higher, as some patients do not seek medical assistance. Most of these cases have no detectable cause.

What are we going to feel, how do we figure out what’s going on, what should we do and when?
Sudden deafness, even in the case of ruptured ear membranes, almost never involves pain in its clinical manifestations. The main symptom is hearing loss in one ear, which subjectively can be felt as a feeling of fullness , or more simply as a numbness. A lot of attention is needed here, in order to prevent the attribution by ourselves of this block to other simpler situations, such as the blockage of the acoustic canal from a wax plug. Hearing loss can be accompanied by 50% dizziness or vertigo (= feeling of rotation), which can vary in intensity and duration.
This vertigo may be accompanied by nausea, a tendency to vomit or even uncontrollable vomiting. In the water it is a very dangerous situation. It can lead to complete loss of orientation and risk of drowning. Easy to say and hard to do, it is necessary to keep cool. The disposal of the weight belt, the expulsion of some air bubbles and follow them to the surface and, above all, the on-time intervention of our guardian angel,our diving buddy, can be life-saving.
Dizziness may stop after we have surfaced, persist or decrease, leaving behind a slight feeling of instability. It can be accompanied by 70% of ear wheezing. It can also be aggravated by head movements or vigorous physical effort as this exacerbates the loss of the lymph. Immediate and complete cessation of physical activity is required, lying down as soon as possible with the head in a higher position than the torso and examination by a specialist at most in 24-48 hours.
The medical examination is statistically more likely to take place when the vertigo is present, because it is a noisy symptom that frightens and awakens us. We should not delay our visit to a specialist when our ear congestion persists for more than a few hours, even in the absence of dizziness and whistles. That’s because the chances of a full recovery of our hearing increase dramatically if special treatment begins within the first 24-48 hours after the onset of symptoms and these are gradually reduced to virtually zero after 14 days. Of course, there is no absolute rule in medicine, which is why treatment is applied even in cases that occur after this period of time.
During our visit to the doctor, it is of crucial importance to make it absolutely clear that we are free divers and to thoroughly analyze the circumstances under which the incident occurred. This man’s contact with the sea can range from rudimentary to non-existent. On the other hand, otoscopic findings may not only be absent, but may be completely misleading and lead to misdiagnosis.
The image of a drum that has been in contact with seawater for several hours often resembles the image of otitis externa or otitis media, which is also mistaken for hearing loss, which can lead to incorrect treatment and tragic loss of time. The sometimes unfavorable conditions under which heroic and distressed doctors of the National Health System are called to practice heroic medicine and the lack of tools and means can catalyze the catastrophe, despite good intentions.
Let yourself be suspicious, based on the knowledge you just acquired. Require and receive at least one audiogram and a tympanogram, which can safely diagnose abrupt deafness. Do not present counter-arguments to your doctor’s recommendation for treatment in a Hospital or Clinic. The global literature is full of studies, which clearly demonstrate the superiority of intravenous drug administration over oral intake at home. Excuses for time limits that pressure us, pale in the face of the argument of increased probability of restoring our precious hearing, even if God has gifted us with two ears instead of one. Hospitalization can last up to 7-9 days.
If the condition does not seem to improve after the first few days, the possibility of applying hyperbaric oxygen therapy, i.e. the administration of oxygen-enriched air at the pressure of some atmospheres, in a special compressed chamber may also be discussed. The rationale is to give plenty of oxygen to the nerve cell that is trying to recover. This is in line with the general principle of the Hippocratic saying “benefit or not harm” which means that if it fails to help us, it will certainly not harm us and at least benefit our skin. Some researchers have suggested that intravenous drug administration through an incision in the eardrum has not proven clear superiority and should be avoided in divers as the procedure weakens the tympanic membrane.
In cases where there is a suspicion of rupture of the ear membranes, surgery may be required immediately to check and seal the window before the inner ear loses all its fluid and dies. The decision to perform surgical repair of a wide rupture should be made immediately within the first few hours of the incident.
Treatment continues at home for about two weeks after leaving the Hospital or Clinic. Complete abstinence from diving and intense physical activity, but also from salt in our diet for at least a month, are considered to be self-evident and even more when surgical treatment has been applied.
Our doctor is the one who will decide the time of our return to the sea.
ATTENTION!
Finally, let us not forget that the restoration of our hearing depends not only on the early diagnosis, but mainly on the prompt onset of appropriate treatment.
Undersea and Hyperbaric Medicine (UHB) – Eustachian Tube – Diving Medicine
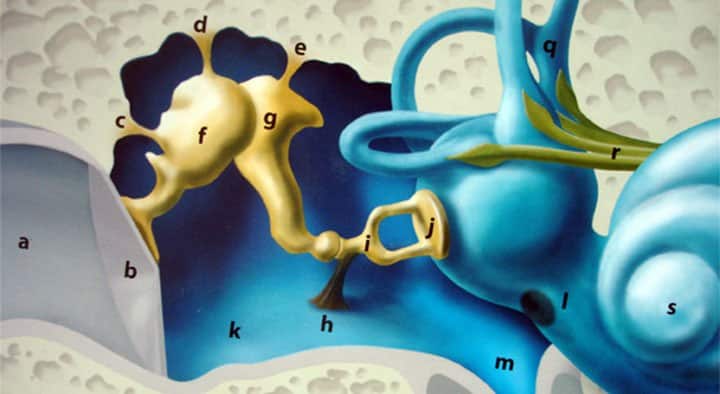
Thus in the fluids of the inner ear there is a pressure of 2 atm. This 1 atm difference is capable of causing the rupture of the inner ear membrane (l) , known as round window. Tearing of this membrane is one of the worst forms of barotrauma. It causes abrupt dizziness with a strong feeling of rotation, loss of orientation and risk of drowning, while it has severe effects on our hearing ability. This subject is of great importance so we will dedicate an entire article to it in the next issue.
If we equalize the air in the middle ear to avoid rupture of the round window membrane, then the difference of pressure on both sides of the drum is capable of tearing the drum from inside out. The same thing can unfortunately be caused, if instead of an earplug, the external auditory canal is blocked by a large amount of ear wax. That’s the reason why divers should occasionally have their ears checked up and, if necessary, have them cleaned.
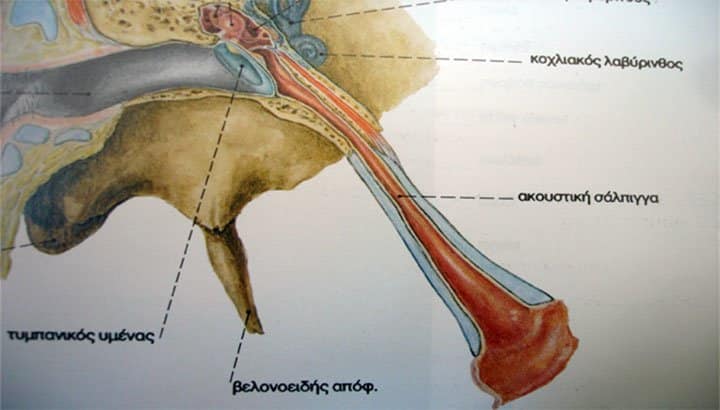
What makes our Eustachian tube work occasionally at its leisure and not as an expensive Swiss watch, as we would definitely like? This tube is the secret key for accessing the magical underwater world. Without it our dives could not go more than 2-3 meters in depth.
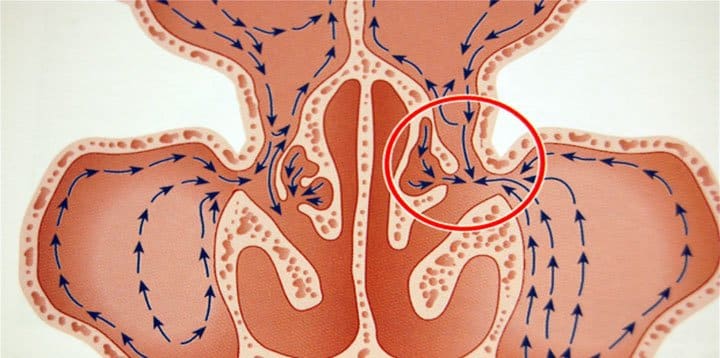
The Eustachian tube has a narrow lumen through which we are called to drive air into the middle ear. This lumen is dressed in a lining (like a wallpaper), called mucosa, and is so narrow that if the lining swells for any reason, it immediately clogs, blocking the airflow inside it. The mucous membrane (gr : vlenogonos), as his name eloquently testifies ( immortal Greek language!), produces mucus (gr: vlena+geno=give birth). The mucus gets spread on it like butter on our bread and should, ideally, be thin enough to allow one sheet of the mucosa to glide easily over the other, at their points of contact. This is precisely what happens in the nasopharyngeal orifice of the Eustachian tube, which is flattened and the sheets of the mucosa touch each other. If mucus becomes dense and sticky, the two sheets are difficult to separate from each other and thus the opening of the orifice becomes difficult to impossible. The same can be caused when thick and abundant mucus plugs mechanically clog the mouth. In other words, goodbye equalization.
What do we do then? Do we blow to unblock the ear? No! Because then we run the risk for serious barotrauma. And since barotrauma is not the subject of this article, but we will refer to it extensively another time, I would just like to dwell on the following:
So let’s just say we managed to open the tube, we even managed to get the fish and we happily start our emergence process. Have you thought that the air we forcibly squeezed into our ear should normally passively escape towards our Eustachian tube? What if she digs in after what we’ve done to her and stubbornly tightens her legs? That’s the moment when laughter and joy stop and difficulties begin. Don’t forget that we are free divers and time is precious- we have to return to the surface! However, the air expands non-stop with our ascent and if it fails to open our Eustachian tube, it will try to intercept any convenient point in its way. And then we say goodbye with tears the integrity of our tympanic membrane, or that of the round window. In a subsequent article we will analyze how serious this situation can be.
What could we do in such a case? In this difficult time it takes experience and cold blood to interrupt the ascend and give time to the air, to leave through the malfunctioning Eustachian tubes, avoiding the worst case scenario. Of course, this, apart from experience and composure, also requires outstanding performance. So here’s another good reason, which explains why we should never approach the limits of our capabilities and why we should never push our equalizations. And which are the situations that make our equalizations difficult?
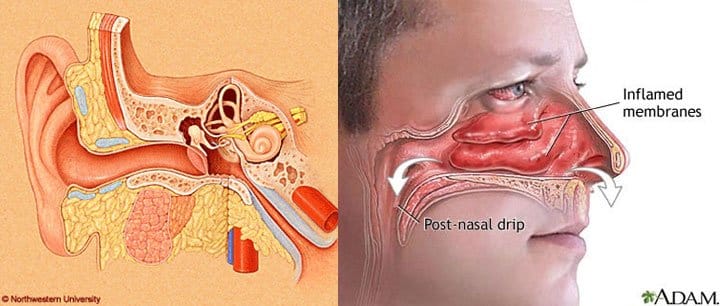
Inflammations of all kinds, both acute and chronic, of the nose, the nasal passages and the nasopharynx. Rhinitis, viral (such as the common cold), microbial, allergic or vasomotor, which with the swelling of the mucosa and the increase in the amount and density of nasal secretions, cause all the above. Sinusitis, ethmoiditis, spenoiditis and forehead sinusitis, which with their irritating secretions floods the nose and of the openings of the Eustachian tubes. Pharmaceutical treatment is imperative and equally requires our short-term abstention from the liquid element.
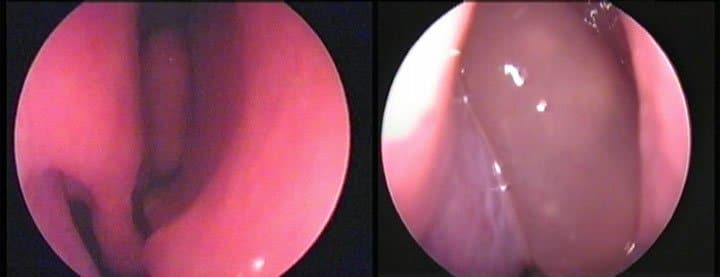
Anatomical problems, such as a deviated nasal septum, hypertrophic inferior turbinates, nasal polyps, chronic sinusitis, hypertrophic adenoids, can easily and painlessly be detected with the help of modern endoscopes for sake of an Eustachian tube that malfunctions. Equally easy and painlessly, with the contribution of endoscopic surgery, they are permanently corrected, restoring the linear flow of air into the nose, the smooth movement of mucus towards the pharynx and the gradual mucous membrane deflation.
Smoking and systematic exposure to urban and industrial pollutants, solvents and chemicals, have a long term effect, in about the same way, causing irritation of the mucosa, swelling and production of abundant, sticky mucus, while in addition, they first paralyze and then destroy the ciliar epithelium of the mucosa, which has the mission of transporting it. It is not easy to change work, especially during the current crisis, but it is sometimes imperative to wear a mask, wash your nose immediately after work and, of course, do not smoke!
The daily nose rinses with saline is highly recommended to everyone. The daily removal of pollutants and microorganisms that accumulate in the nasal mucus can not only have positive benefits for our body, but also benefits for the better functioning of our Eustachian tubes.
Particular attention should also be paid to the importance of consuming plenty of water before, but especially during our dive. Keep in mind that water takes at least twenty minutes until it reaches the nasal mucous and hydrate it. Since the sensation of thirst diminishes during diving and will therefore not alert us, it is advisable to drink water at least every half an hour, even if this increases our urination. The water we drink should be at ambient temperature and not frozen, because it will then shock the mucous membranes, causing swelling and increased mucous production.
To sum up, the proper functioning of the Eustachian tube requires the absence of inflammatory factors or anatomical problems. If they are missing and with the proper training, everyone can succeed. However, in the most difficult cases, training should be done without a speargun in our hands, in order to put all our attention to equalization maneuvers.
Finally, I would like to close with a personal piece of advice. Do not hesitate to postpone, in the slightest suspicion of cold or allergy, the anticipated fishing trip that you have been planning for so long. Underwater hunting is a demanding activity, which requires the proper functioning of all our organs and organic systems and does not bear compromises.
Undersea and Hyperbaric Medicine (UHB) / Diving Medicine – Frontal Balloon Sinuplasty
One theory says that they exist to reduce the weight of the head, while a second says that they function as voice resonators. This may explain why the voice changes so much in case of sinusitis, as the sound of a guitar would change if we filled its resonance with paper.
The orifices and pores are necessary in the nasal cavities, so that the air that exists within them can circulate freely and be recycled, but also to discharge the secretions produced by the mucous membrane that covers them.
It is very likely to cause mucosal rupture and bleeding inside the sinus, which in addition to the intense pain, will be perceived as nose bleeding to the mask. If the blood cannot be excreted and remains into the sinus, it causes the development of thick mucus, cyst or polyps.
The situation should immediately be dealt with and for a sufficient period of time, as this will be indicated to us by the specialist. The display of disregard, which could under certain circumstances be forgiven to a land creature, is unforgivable though by the aquatic part of our amphibious character. We should not leave the situation become a chronic condition, because that will certainly lead us to surgery.
And if we don’t avoid it and get to that point, what kind of surgery will it take?
Sinus surgery has experienced a revolutionary progress within the 2-3 past decades, with widespread use of surgical endoscopes. The reliable and safe use of various endoscopic surgical instruments, has provided a wonderful solution to the problem of obstruction of the orifices of the paranasal cavities.
The frontal sinus, however, has remained distant for the endoscopic surgeons, just like the dentex for the average hunter. It is undeniably a difficult surgical field, with rugged paths, and respectable proximity to the delicate structures of our skull, such as the brain. As an undesirable negative factor in the long-term patency of the enlarged orifice of the frontal sinus, the unexpected accumulation of post-operative scar tissue has almost always remained. This, especially in the case of the frontal sinus with the narrow and long canal, increased the likelihood of slowly or rapidly leading to recurrence and reappearence of symptoms. The only solution would be to enlarge the orifice with minimal trauma and maintain as much mucosa as possible so that the necessary function of the mucosal epithelium is maintained.
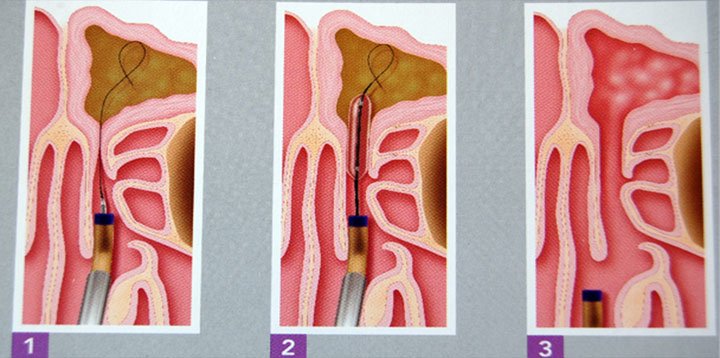
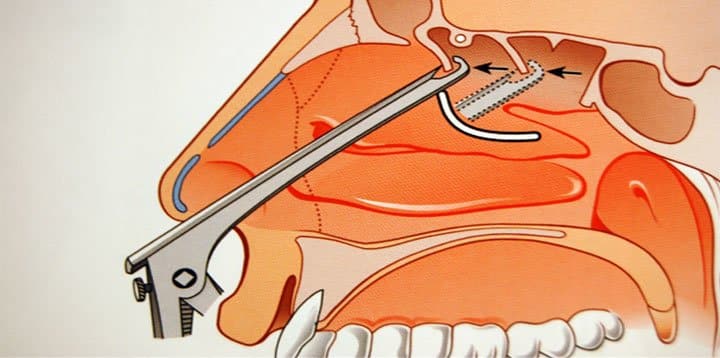
The philosophy and technique is simple. A thin wire, which has an optical fiber with led light at its end, is inserted with the help of an endoscope into the frontal sinus. With the wire as a guide, the special balloon is forwarded through the orifice into the sinus.
When the balloon reaches the height of the narrowed orifice, it is filled with low-volume, high -pressure air, so as to break the thin bony diaphragms of the cells that narrow the lumen, fully respecting the mucous membrane. The whole procedure lasts a few minutes and can also be done with local anesthesia, if the operation is individually related to the frontal sinus. It can also be applied to all paranasal sinuses, while it can finally be combined with conventional (ESS) or functional (FESS) endoscopic sinus surgery, under general anesthesia.
A big advantage is that, if applied individually to the frontal sinus, the patients can return to their normal activities the next day and a few days later to underwater hunting.
As a method, it has been in use since September 2005. The results, which now talk about 12 years of postoperative monitoring, give rates of orifice maintenance, which ranged in the various studies from 80% to 90 %, rates considered by the World Medical Community, to be completely acceptable and have highlighted the method as one of the most important weapons in modern surgery.
The method has been applied in our country since 2008, with excellent results. Approval is expected for the material to be granted by National insurance funds of our country (it is already provided by private insurance), so that it can be applied to the entire population.
It is undeniable that we are experiencing a difficult global situation. The crisis, artificial or not, knocks on everyone’s door. What makes it so beautiful today is access to an endless source of knowledge and the development of technology, which in good hands and for noble purposes, equips us with so many magical possibilities to prevent the impossible.
Equalization Methods – Spearfishing
The hottest topic, when one starts discussing the problems of his underwater life, is the equalization of pressure on his ears during diving.

Mother Nature didn’t have in mind air travel and scuba diving when she created us. If she had thought about it, she would absolutely have sent the original model of Eustachian tube back to the R&D dept. Rapid vertical movement is a human achievement, and the energetic equalization of the great change in pressure in the aerial cavities of our bodies is a little out of our nature. However, with the use of advanced techniques, almost everyone can make ear equalization much easier. We have analyzed thoroughly in previous articles the Eustachian tubes, their anatomy and their problems.
Let’s get to know the methods of equalizing the pressure in our middle ear today.
The Valsalva method
Antonio Valsalva was the first to describe in 1704 a procedure for equalizing pressure in the middle ear. The method is the following: we close our nose with the index finger and the thumb and exhale air from the chest. Our cheeks should not swell and the effort should be fast and not too intense. The air compressed by the contraction of our expiratory muscles through the open glottis (= our genuine vocal cords located in the larynx) will be directed through our Eustachian tubes into the middle ear. It is the simplest and most widespread technique among free and independent divers and the most feasible for the novice diver. But this method has two main disadvantages.
The first is that the increase in exhaled air pressure causes an increase in blood pressure in the veins and edema in the tissues around the Eustachian tube.
The second is that this increased pressure on the chest reduces venous blood flow to the heart by affecting blood pressure and heart rate. For these reasons, early alternatives of equalizing were sought early on.
The Frenzel method
Herman Frenzel was a military doctor, an ENT surgeon who monitored Luftwaffe pilots during World War II. He invented the homonymous technique in 1932 and instructed pilots of the Stukas bombers, who by applying a vertical onrush on the target to accurately direct their “dumb” bombs, experienced rapid changes in barometric pressure, corresponding to those of diving. The technique is based on the closure of the glottis, the vocal cords, such as when it comes to lifting a heavy object. The index finger and thumb close the nose and we try to get a laryngeal sound that sounds like “kh” or “”g”. In this way, the rear part of the tongue rises upwards and back, pulling the larynx upwards and pushing air like a plunger into the Eustachian tubes. For this reason the method is also called “throat piston” . To practice it, it is enough to observe the sides of our nostrils swell over our fingers that close the entrance to the nose and see the Adam’s apple in our throat descending like a plunger. It is the best of the air pressurization equalization methods. It is easy to achieve with a little training and does not prevent the venous return of blood to the heart.
The Toynbee method
In 1853, Joseph Toynbee was the first to recognize the sound in our ears during swallowing as a result of air entering the middle ear from the Eustachian tube, which had been described much earlier, in 1574, by Bartolomeo Eustachio.
The method he described was simple. It consisted of closing the nostrils with the fingers during swallowing. The muscles connected with the swallowing process pull and open the mouth of the Eustachian tube. At the same time, the air that is compressed by the rise of the larynx when we swallow does not leave our nostrils, because we block them with our fingers, but it is directed towards the tubes. Of course, this method of swallowing air is difficult to be repeated , especially in the case of a novice diver.
The Lowry method
It is a combination of Valsalva and Toynbee methods. We close the nose with our fingers, exhale air from the chest and swallow at the same time. It is a technique that can be used if Valsalva alone does not prove to be effective, so some divers prefer it.
The Twitch method or head tilt method
It is another combined method of equalizing with air compression. It combines the Valsalva or Frenzel maneuner, no longer by swallowing, but abruptly tilting the head to the left and right, so that the tension of the pharyngeal muscles facilitates the opening of the Eustachian tube.
The Beance Tubaire Voluntaire (BTV) method
This method of voluntary opening of the mouth of the Eustachian tube was developed in 1952 by the French Navy. It is a difficult method to teach, and of those who try to learn it only 30% can achieve it with stability and reliability. The technique is based on contraction of the muscles of the soft palate (it is the soft membrane behind our palate that ends in the uvula) while pressing the lower jaw forward and down with the mouth closed. It’s like trying to yawn kindly at a boring event without being perceivable. When achieved, the characteristic “click” of the opening of the mouth of our Eustachian tubes is heard. It is a method that does not require the closure of the nostrils, so we do not waste our hydrodynamic shape during diving but also do not keep our hand busy. If we get used to it, it is a great method that can help keep our muscles constantly contracted and the equalization is done automatically as we descend or repeatedly and continuously. Some people look like they were born with this talent, but for others it’s the result of systematic training.
The Roydhouse method
The method was described by Noel Roydhouse, a New Zealand doctor, and is a variant of BTV. It is a voluntary contraction of the muscles of the soft palate in such a way that the uvula is towed up and forward, which can be practiced in front of a mirror. If this is achieved, we have learned 50% of the method. The rest is about contracting the muscles of the tongue and jaw, in a way as if we are trying to make smoke rings.
I have never made my own tobacco rings, nor do I suggest that you start smoking. But try, if you wish, with the mouth open in the mirror, to see the uvula moving up and forward first, and then with jaw and tongue movements listen to the characteristic ‘click’ in your Eustachian tubes. I would certainly recommend not doing all this in the presence of others. We don’t want to put our loved ones in the process of wondering about our mental health.
The Edmonds method
Carl Edmonds, an Australian author, described a method similar to BTV (soft palate and tongue muscle contraction) combined with forward jaw movement and flexion of the throat with or without Valsalva or Frenzel. All of them aim to the disposition to open of the mucosa and muscles around the mouth of the Eustachian tube.
A prerequisite for applying all these is to be free of upper respiratory infections, allergic rhinitis and also be well hydrated.

Blocked Ear After The Diving

We come out of the sea after the coveted dive and the ear feels blocked, with or without pain, with or without a whistle or dizziness. And now what?
Our next moves are usually determined by the severity and duration of our symptoms, but also by our temperament. Most likely, the pain, the whistles and dizziness, especially if they persist, will surely lead us to a specialist for help. But what about the humblest of symptoms, ear blocking?
We often underestimate the symptom and negligently contribute to permanent ear damage. So this blocking can be something very innocent (such as earwax that doubled its volume from the water and blocked completely our external acoustic canal), or something very serious. If it disappears on its own, at least a few hours after our dive, everything is under control if all the other symptoms are absent.
This means that we must, at least, control our hearing ability, which should not be lacking on this side, compared to the other ear. We can check that, by swapping our cellphone between our two ears.
If the feeling persists, sleeping over the problem and be like “ok brother, let’s see tomorrow how it goes” is not always the best option. Conditions such as rupture of the eardrum, secretory otitis (fluid collection in the middle ear), otematoma (blood collection in the middle ear), rupture of the round window membrane (we could talk about it for days and we will certainly do so) and sudden hearing loss, are possibly just outside our door. All the above are serious issues and have been reported in an increasing order of importance, all of them need treatment, but the latter two are medical emergencies and must be treated within the first hours by a specialist who has knowledge in diving issues. The earlier the treatment begins the better for the final outcome. If we decide to deal with the matter days or worse, weeks later, then goodbye my precious ear, and how good you were when I had you and how much I’m going to miss you and stuff like that.
Another subtle and slightly annoying issue is that in some cases the outcome is negative, even though patients have visited a doctor. There are various reasons for this misfortune. Either the patient fails to explain the exact situation that has led to the symptoms, or the doctor cannot interpret them properly, or due to the fact that conditions do not allow them to devote the time they wish, or the doctor does not have the necessary equipment (at least one tympanogram and an audiogram need to be conducted immediately). In addition, for many people, even ENT experts, the marine environment and its effects are terra incognita. How often is it, when you declare that your hobby is spear fishing, that the first question you receive, with an emphasis of certainty, is : “with scuba, huh”?
Concluding with some messages to remember: A blocked ear, always demands our attention after getting out of the water. If there are more symptoms, such as pain, dizziness or humming, we should definitely visit a specialist. If numbness as a sole symptom persists, more than a few hours, we should not neglect to check it out, because even if God assorted the ear into the binary organs, we need both of them to enjoy our precious, high-fidelity stereo system.
Seek specialized advice, any time of the day or night, because integrity in all our organic systems is a prerequisite for engaging in such a demanding and beloved sport.
Undersea and Hyperbaric Medicine (UHB) / Diving Medicine- Paranasal Sinuses
Barotraumas of Paranasal Sinuses
The paranasal sinuses are spaces filled with air inside our head and their mission is mainly to serve as voice resonators, as the prevailing theory argues those who try to interpret their existence.
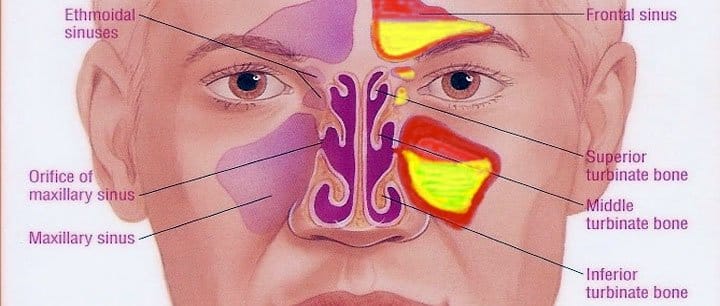
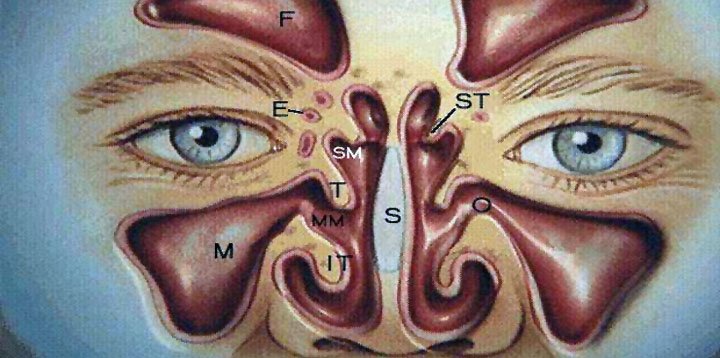
These cavities are usually symmetrically placed on either side of the middle line of our face and are the maxillary sinuses (located in our cheeks), the ethmoid air cells (located between the nose and eyes), the frontal sinuses (located in the area of our eyebrows and forehead) and finally, the sphenoid sinuses (located in the center of the head behind the nose).
To get a better picture, imagine the nose as an elongated corridor, where air circulates. On the right and left of the corridor, are symmetrically placed small and larger rooms, the paranasal sinuses.
Each of these rooms communicates with the corridor, not with a large door, but with a small window. The rooms, as well as the corridor, are covered with a lining (wallpaper), which is called mucous membrane. The windows are so narrow that if the lining swells for any reason, the airflow between the rooms and the hallway is significantly reduced or completely stopped.
Without air and a window, the rooms cannot be cleaned, they collect dirt that is contaminated by microbes in the area. The festival of inflammation has begun and its ending depends on many parameters. One of them is our attitude towards this situation.
When we suffer from a common allergy, allergic rhinitis, sinusitis (or rhinosinusitis in general), our nose is blocked and produces more secretions than usually does. The mucous membrane (the wallpaper) is edematous and the orifices of the paranasal cavities are blocked. If we attempt to dive into such a situation, we will have to confront another degree of difficulty in equalizing the air pressure in our paranasal cavities.
This will initially look like a feeling of pressure on the face, which gradually increases as our depth increases and gives way to pain, which can often be very intense. Depending on the affected area, we feel pain in the cheeks or teeth of the upper jaw, in the root of our nose, or between the eyes, the eyebrow or forehead or the center of our head. If we persist trying and don’t cease diving, one of the following things can happen:
1. The air may eventually be able to equalize the pressure in the sinus and come out of it during the ascend with no damage.
2. The air fails to penetrate the blocked orifice. This results in a drop in pressure into the sinus as the depth increases, leading to vessel rupture and bleeding.
3. The air can ultimately penetrate the narrowed sinus and gets trapped there, so that it does not automatically exit during ascend. This phenomenon is known as reverse block. Due to its dilation, it will at some point exceed the elastic limit of the mucosa that creates the valve, with subsequent tearing and bleeding into the sinus and nose.
These two aforementioned forms of barotrauma of the paranasal sinuses, the barotrauma of descent and that of the ascend, can put us in trouble, temporarily or permanently.
With proper medication and abstinence from diving, we must ensure that blood is drained, the mucosa membrane decongested, the orifice open and air circulation restored between the nose and the sinus.
This intervention should not be delayed for long, nor should the situation be left to the possibility of auto therapy without doing anything because the only thing we would possibly achieve would be to turn this situation into chronic. More serious complications are, fortunately for us, very rare. As creatures that dive, however, we risk something far more important. Our ability to continue to dive.
Inflammation in the mucosa of a nasal cavity leads to hyperemia and subsequent hypertrophy, which can become permanent. This means that the cavity, instead of a thin lining, is now coated by a thick carpet, which in places often has extra thicknesses, cysts and benign masses, called polyps.
If these formations are away from the orifice of the sinus, the situation can exist for years, without being realized and without making it difficult for us to dive. If it occupies part of the orifice or completely blocks it, it causes correspondingly greater equalization problems.
In addition, this edematous mucosa, which is located near the orifice without blocking it, can cause a disproportionately large blockage of the orifice, even with a simple cold that would be undetected on others. In other words, the orifice of the sinus will close for the slightest reason, exposing us to the risk of barotrauma.
All of these are not meant to scare or annoy us, but to let us understand the following. Those of us who dive or do an intense sporting activity are required to have perfect functionality of all of our organs in order to perform a sequence of actions that require perfect coordination. Discounts and bargaining do not fit in here. A small factor that might be overlooked or underestimated can cause a chain of reactions with unforeseen consequences.
If we owned a submarine, even a small low cost one, we would never start a dive, knowing that one of its systems sometimes malfunctions, or is simply unreliable. So let’s think about our body’s incalculable value, which is the “ship of our soul and existence”.
With the help of endoscopic nose surgery and paranasal cavities, we can safely remove all of this pathology today, widen the orifices, trim the gaps between the rooms and create uniform, comfortable and well ventilated air cavities. All this can be done without major hospitalizations and most importantly, with almost no pain. After a period of 3 to 8 months of necessary abstention from the sea for recovery, the problem in the vast majority of cases is finally resolved.
This, of course, does not mean that we are entitled to relax our self-protection measures. It is known that there is no better cure than prevention. No matter how good the attempt to restore a problem is, it cannot be more efficient and ultimately preferable than trying to prevent its appearance.
The Messages of Our Body
Summer is rolling, excruciatingly fast to its end, giving way to a sweet, slightly melancholic but clearly better, from a diving and fishing point autumn, in my humble opinion. And it is the time when the sea clears out of these foolish and reckless guys who show-off and slalom among our buoys and that is already enough for me.
The other day, I was fishing in a deep part of the sea, just fifteen meters from the vertical wall of the coastline. While I was looking for fish, a terrifying and incredibly close noise of a large outboard froze me. I hurried to cling on the rock and climbed to the surface as slowly as I could. I had time to see, but unfortunately not to stop, the unbelievable person who was speeding away giggling, having just passed between the vertical rock and my buoy. I’m not describing anything new, of course, but anyone who has faced a similar experience can guess how much time I trembled with fear and anger.
Monday
17:30 – 20:30
Tuesday
17:30 – 20:30
Thursday
17:30 – 20:30
27 Marathon Avenue
Pallini, 15351
Tel: 2106614140

Για πολλά όμορφα αποτελέσματα ρινοπλαστικής, ακολουθείστε μας στο Ιnstagram!
